Cancer
People living with cancer deserve treatments that are tailored to their unique circumstances. We know that because we’re focused on discovering the medicines that can have the greatest impact on some of the hardest-to-treat cancers. The medicines that unequivocally show early signs of progress will matter most to the people with the disease.
Whether it’s treating rare tumor types, leveraging precision medicine, or finding new treatments for those with limited options, we’re constantly in search of ways to make life better for people navigating cancer.
Looking for financial assistance? The Lilly Support Center is available to provide financial assistance information for those prescribed a Lilly Oncology product. You can visit lillyoncologysupportcenter.com or call 866-472-8663, Monday-Friday, 8 a.m.-10 p.m. (Eastern time) for more information.
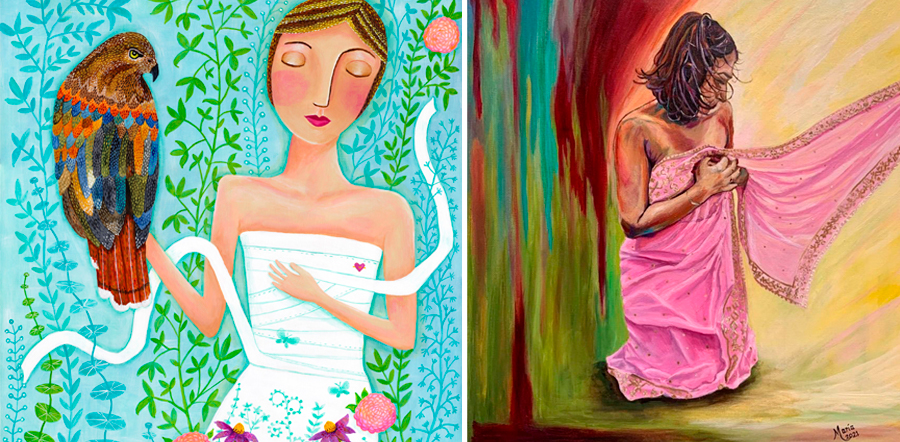
Oncology on Canvas®
For two decades, Oncology on Canvas® has provided people in the cancer community an opportunity to share their stories through art and narrative. The program, a partnership between Lilly, the National Coalition for Cancer Survivorship and the Cancer Support Community, serves as a creative outlet for patients, their loved ones and their care teams. Originally a competition, the program encourages submissions of all types, including poetry, watercolor; oil and acrylic painting; pastels; photography; and mixed media artwork. You don’t have to be a professional artist to experience the power of creative expression. Share your story today.
Oncology on Canvas® Art Gallery
Creative expression is more than just an outlet. It's a way for anyone affected by cancer to inspire hope.
View the Art Gallery